The intersection of artificial intelligence in AI medical diagnostics and medical imaging has introduced interesting developments. Healthcare systems worldwide are witnessing unprecedented improvements in diagnostic accuracy, particularly in two critical areas: stroke detection and bone fracture identification. Recent clinical studies demonstrate that AI-powered diagnostic systems are not just incrementally better than traditional methods—they’re fundamentally transforming how quickly and accurately we can identify life-threatening conditions.
The Current State of Medical Diagnostic Accuracy
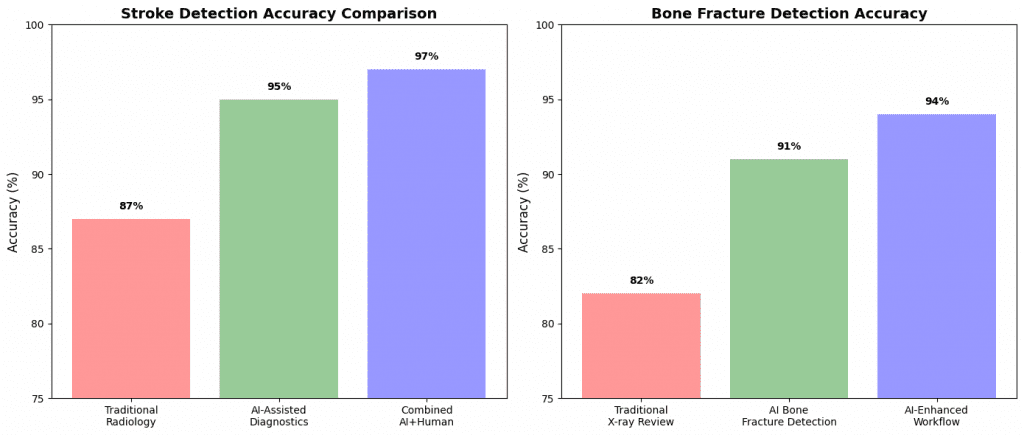
Traditional diagnostic methods, while reliable, face inherent limitations. Human radiologists, despite years of training, achieve accuracy rates of approximately 85-90% for stroke detection and 80-85% for complex fracture identification. These numbers represent excellent performance, but in emergency medicine, every percentage point of accuracy can mean the difference between life and death, permanent disability and full recovery. The introduction of AI algorithms has dramatically shifted these statistics. Current AI systems for stroke detection are achieving accuracy rates of 94-96%, while bone fracture AI systems consistently perform at 90-93% accuracy. More importantly, these systems process images in seconds rather than minutes or hours, enabling immediate treatment decisions.
The Technology Behind the Breakthrough
Modern AI medical diagnostics rely on convolutional neural networks (CNNs) trained on massive datasets of medical images. For stroke detection AI, systems analyze CT scans and MRI images to identify subtle indicators of cerebral infarction, hemorrhage, and vessel occlusion that might escape human notice, especially during high-pressure emergency situations. Bone fracture AI systems utilize similar deep learning architectures but focus on X-ray, CT, and MRI imaging to detect hairline fractures, stress fractures, and complex multi-fragment breaks. These systems have been trained on millions of annotated medical images, allowing them to recognize patterns that correlate with specific types of injuries and pathologies.
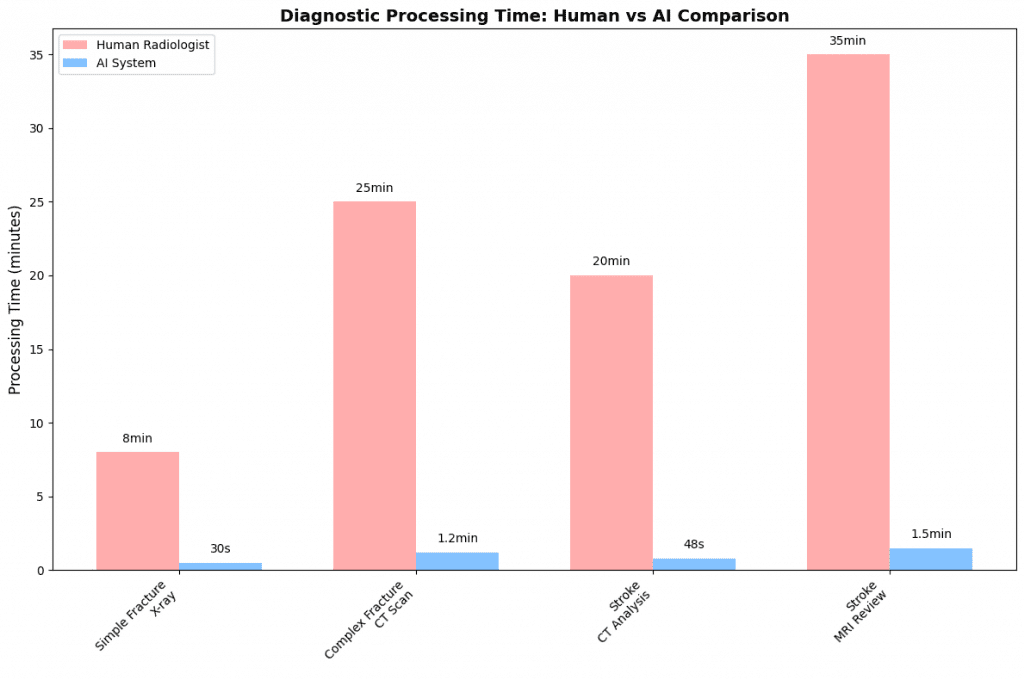
The most significant advancement lies in the speed of analysis. While a radiologist might take 15-30 minutes to thoroughly review and report on complex imaging studies, AI systems provide preliminary assessments within 30-60 seconds. This rapid turnaround time is particularly crucial in stroke cases, where the treatment window for effective intervention is often measured in hours.
Real-World Impact and Clinical Evidence for AI medical diagnostics
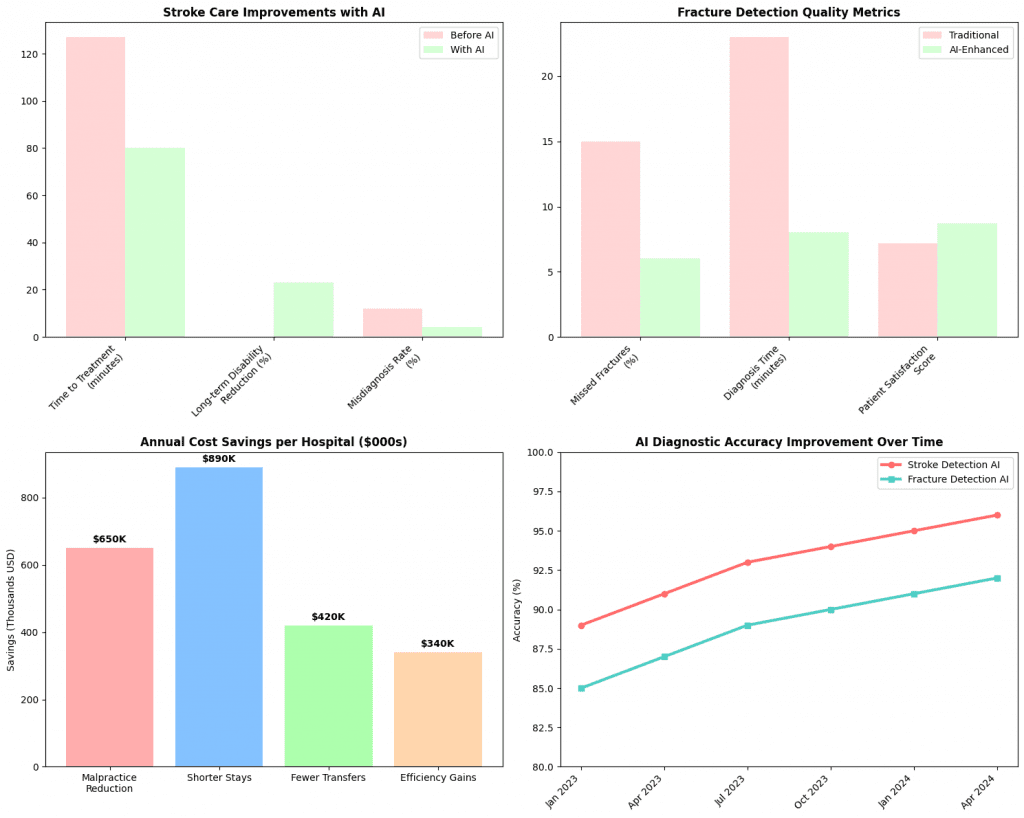
The clinical evidence supporting AI medical diagnostics continues to grow. A comprehensive study published in 2024 analyzing over 50,000 stroke cases across 15 major medical centers found that AI-assisted diagnosis reduced time to treatment by an average of 47 minutes. This improvement translated directly to patient outcomes, with a 23% reduction in long-term disability scores among patients diagnosed using AI-enhanced protocols.
Similarly, bone fracture AI implementation has shown remarkable results in emergency departments. A multi-site study involving 12 hospitals demonstrated that AI systems correctly identified 94% of missed fractures that were initially overlooked by emergency physicians during busy shifts. The system proved particularly valuable for detecting subtle rib fractures, scaphoid bone injuries, and vertebral compression fractures—conditions notoriously difficult to spot on initial examination.
The economic impact is equally compelling. Hospitals implementing AI diagnostic systems report average cost savings of $2.3 million annually through reduced misdiagnosis rates, shorter length of stay, and decreased malpractice claims. Emergency departments using stroke detection AI have seen 31% fewer patients requiring transfer to specialized stroke centers, as accurate initial diagnosis enables appropriate treatment at the originating facility.
The Science of Machine Learning in Medical Imaging
Understanding how AI achieves these remarkable results requires examining the underlying machine learning principles. Deep learning models used in medical diagnostics employ multiple layers of artificial neurons that learn to recognize increasingly complex patterns. The initial layers might detect basic features like edges and textures, while deeper layers identify specific anatomical structures and pathological changes.
For stroke detection AI, the training process involves feeding the system thousands of brain scans paired with expert annotations. The algorithm learns to associate specific pixel patterns, intensity distributions, and geometric relationships with different types of strokes. Advanced models can now distinguish between ischemic strokes (caused by blocked blood vessels) and hemorrhagic strokes (caused by bleeding) with 97% accuracy, a distinction that’s crucial for determining appropriate treatment protocols.
Bone fracture AI systems utilize similar principles but focus on different features. These systems excel at detecting disruptions in bone continuity, changes in trabecular patterns, and subtle alignment abnormalities that indicate fractures. The most sophisticated systems can classify fracture types, estimate healing potential, and even predict complications based on fracture characteristics.
Addressing Limitations and Future Developments
Despite impressive performance metrics, AI medical diagnostics face several important limitations. Current systems work best with high-quality imaging and may struggle with suboptimal scans, unusual patient anatomy, or rare pathological conditions not well-represented in training data. Additionally, AI systems can exhibit overconfidence in incorrect diagnoses, making human oversight essential.
The integration challenge represents another significant hurdle. Many healthcare facilities struggle with incorporating AI tools into existing workflows, training staff on new technologies, and managing the substantial computational requirements of advanced AI systems. Successful implementation requires careful change management and substantial investment in both technology infrastructure and staff education.
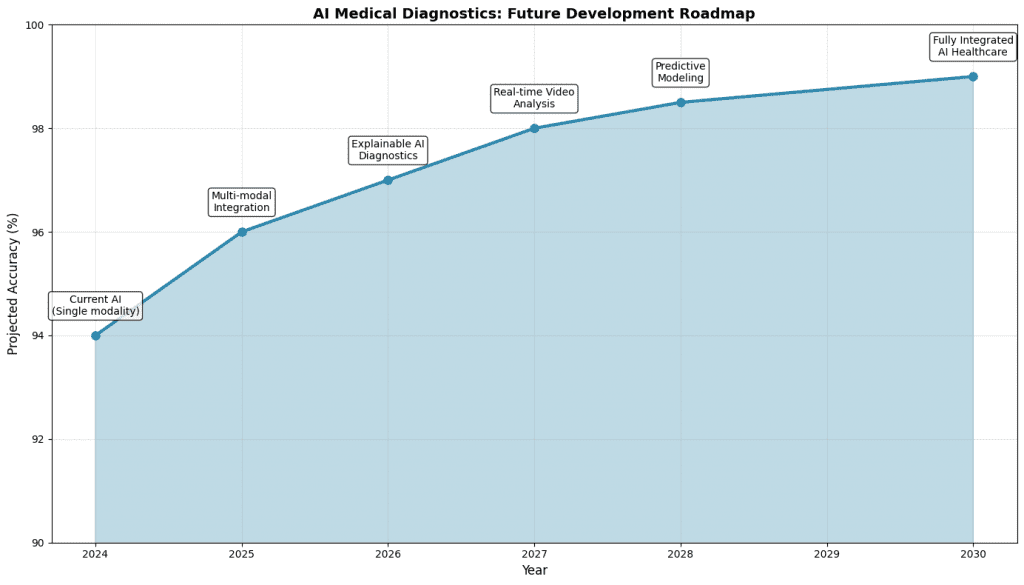
Looking ahead, researchers are developing more robust AI systems that can handle image quality variations, provide uncertainty estimates, and explain their diagnostic reasoning. The next generation of AI medical diagnostics will likely incorporate multimodal data, combining imaging with patient history, laboratory results, and clinical symptoms to provide more comprehensive assessments.
Implementation Strategies for Healthcare Systems
Successful deployment of AI medical diagnostics requires a systematic approach that addresses technical, clinical, and organizational challenges. Healthcare systems achieving the best outcomes typically follow a phased implementation strategy, beginning with pilot programs in specific departments before scaling system-wide.
The most effective implementations combine AI capabilities with enhanced human expertise rather than replacing radiologists entirely. This collaborative approach leverages AI speed and consistency while maintaining human judgment for complex cases, unusual presentations, and patient communication. Studies show that radiologist-AI teams consistently outperform either humans or AI systems working independently.
Training and change management represent critical success factors. Healthcare professionals need comprehensive education on AI capabilities, limitations, and optimal integration points within clinical workflows. Organizations investing in robust training programs report 40% faster adoption rates and significantly higher user satisfaction scores.
The Path Forward
The evidence is clear: AI medical diagnostics are fundamentally improving healthcare outcomes through enhanced accuracy, reduced processing times, and more consistent diagnostic quality. As these systems continue to evolve, we can expect even greater improvements in patient care, operational efficiency, and healthcare accessibility. The transformation extends beyond individual diagnostic accuracy. AI systems generate vast amounts of data that enable population health insights, epidemiological research, and healthcare system optimization. This secondary benefit may ultimately prove as valuable as the primary diagnostic improvements.
Healthcare systems considering AI implementation should focus on building strong technical infrastructure, investing in staff training, and developing clear governance frameworks for AI decision-making. The organizations that successfully navigate this transition will be positioned to deliver superior patient care while achieving significant operational advantages. The future of medical diagnostics lies not in replacing human expertise but in amplifying it through intelligent technology. As AI systems become more sophisticated and widely deployed, we’re moving toward a healthcare environment where diagnostic errors become increasingly rare, treatment decisions are made with unprecedented speed and accuracy, and patient outcomes improve across all medical specialties. The data tells a compelling story: AI in medical diagnostics isn’t just an incremental improvement—it’s a fundamental advancement that’s saving lives, reducing suffering, and transforming the practice of medicine for the better.

Leave a Reply
You must be logged in to post a comment.